Key Takeaways
- Active T cells are an integral part of the body’s defense against pathogens and cancer.
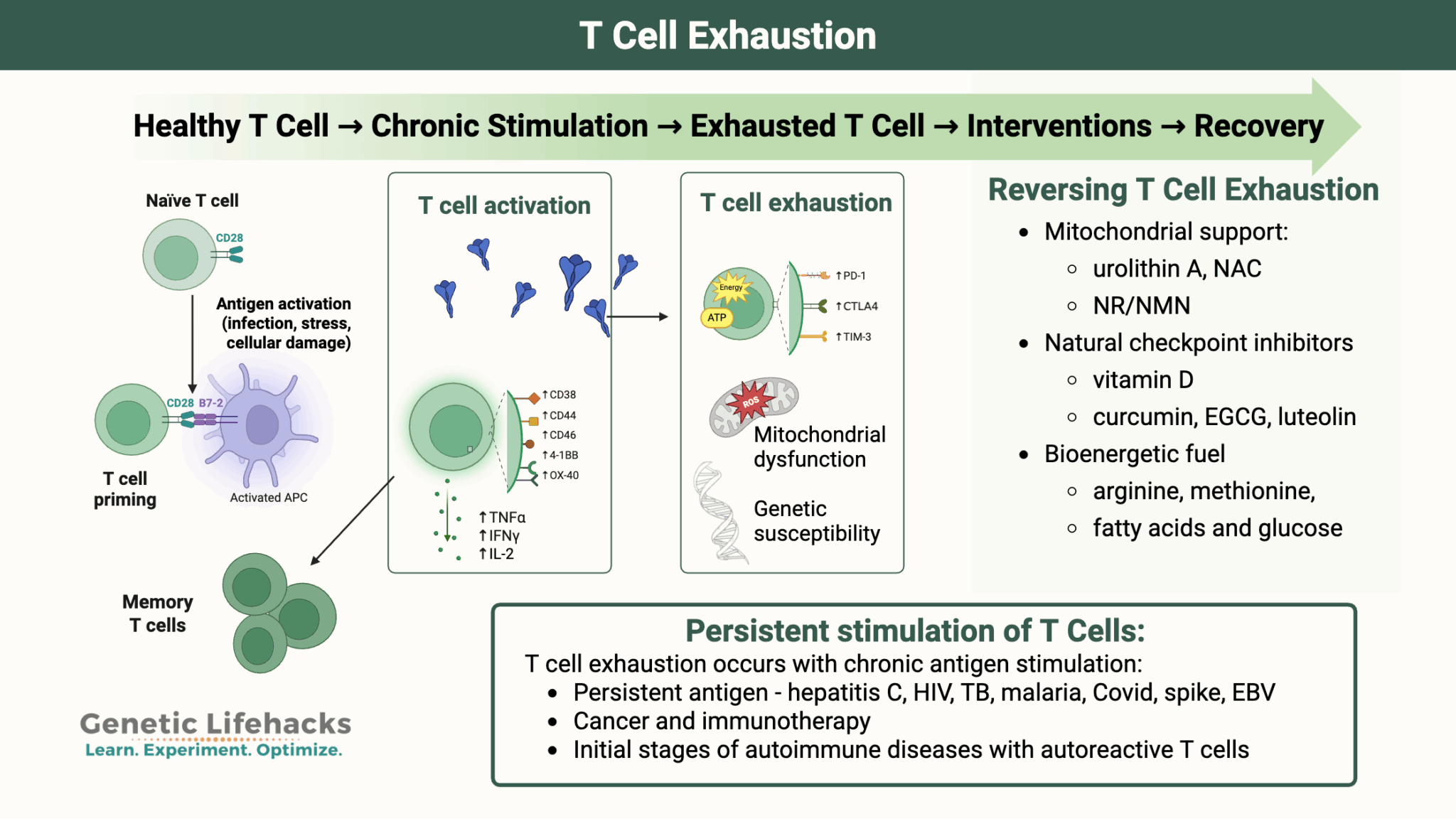
- Chronic, persistent stimulation can cause T cells to go into a state of exhaustion, no longer functioning well enough to protect the body.
- T cell exhaustion can occur in cancer, immunotherapy, HIV, hepatitis C, and possibly long Covid/ME/CFS or vaccine injury.
- Genetic variants play a role in susceptibility to T cell exhaustion.
- In some cases, T cell exhaustion can be reversed by providing the T cells with the right nutrients and blocking the checkpoints.
T-Cell Exhaustion
A few years back, I took a deep dive into how inflammation is resolved, such as after an injury. The resolution of inflammation is an active process that relies on DHA and EPA (omega-3 fats) to synthesize specific lipid mediators that turn off inflammatory signals and restore tissue to normal. When inflammation isn't resolved, it leads to low-level chronic inflammation—the root of most chronic diseases.
This led me to the question: If the resolution of inflammation is an active process (and leads to chronic disease when it is limited), what happens when the adaptive immune response doesn't get resolved?
The adaptive immune response includes T cells, which can fight cancer and destroy pathogens (bacteria, viruses, etc). T cells are activated by antigens, which are particles from pathogens or tumor cells.
But here's the problem: T cell exhaustion happens when your immune system’s T cells get worn out from fighting the same problem for too long -- whether from a persistent viral infection, cancer, or ongoing antigen stimulation.
When stimulated for too long by persistent antigens, T cells enter a state referred to as T cell exhaustion. They lose energy, become much less effective at killing off threats, and don’t multiply like they should. Basically, they’re still around, but their fighter skills are on mute, so your body can’t respond to infections or cancer as it should.
On a cellular level, T cell exhaustion occurs when T cells express lots of “brakes” (inhibitory receptors like PD‑1) that dampen their activity. Their mitochondrial energy supply also sputters, and they generate excess ROS, making it even harder to recover.
The good news? In some situations, T cell exhaustion is reversible by supplying the right nutrients and inhibiting the checkpoints (the receptors that put the brakes on).
How does this connect to long Covid, ME/CFS, lung function, and even mRNA vaccines?
In people with long Covid or ME/CFS, scientists often see T cell exhaustion—possibly because the immune system got stuck reacting to lingering viral particles or inflammation.
A long Covid study showed that T cell exhaustion was seen in patients for months, but by 24 months, some people do recover as their T cells slowly rebound. A minority of people also have similar symptoms post mRNA vaccination, with extended spike antigen production and similar patterns of T cell exhaustion. It all ties back to the idea that when your immune system faces ongoing challenges, your T cells can burn out, affecting recovery and overall immune response.
Lung problems, including COPD and asthma, can also involve T cell exhaustion, which may lead to increased susceptibility to respiratory infections.
Is T cell exhaustion the whole picture for long Covid, ME/CFS, vaccine injuries, and COPD? Probably not -- think of this as one piece to the puzzle. These conditions are heterogeneous and likely have multiple mechanisms involved.
The good news is that there are natural ways to support T cell function (see the Lifehacks section of the new article for a three-pronged approach). Even more importantly, there's a ton of research going on to reverse or prevent T cell exhaustion for cancer immunotherapy, and even a clinical trial using a way of stimulating T cells for long Covid.
Why should you care about this if you don't have cancer or chronic fatigue?
Because immune system dysregulation and T cell exhaustion are also problems in aging. This ties in perfectly with my latest Longevity Lifehacks article on a clinical trial that shifted T cells to a less exhausted state in older adults...
And yes, genetic variants in the T cell checkpoint receptors play a role in susceptibility to T cell exhaustion. It all comes together nicely, which is why I think this is an important topic for many of us!